The first really beautiful summer day of 2017 occurred on the first day of May. A friend and I decided we were going to go hiking – the trail was about 5.5 miles long, with about 500 feet of elevation change. The trail surface was mostly dirt and stable rock so I decided with the warm weather to break out my hiking sandals that I had broken in the previous summer.
On the last descent of about 450 feet, I “blew out” my right foot. Afterwards, I learned that my well ventilated but poorly designed sandals with very little arch support had given me my first introduction to plantar fasciitis.
What is Plantar Fasciitis
Medical websites often define Plantar fasciitis as a common cause of heel pain. In my case, I would expand on that and describe the worst of the pain in the arch of my foot, extending from the base of my big toe all the way to the front of my heel. It was excruciating and, while I could walk, it was difficult and painful. It was worse when I got up in the morning and first put any weight on the foot.
I learned that people who are on their feet for long periods or engage in activities like running and hiking are the most likely to experience it. I had been active and on my feet all my life, so I was really surprised when I got it! I didn’t even know what to call my symptoms until I did some research. Sure enough, I found that the common plantar fasciitis symptoms include:
- Sharp pain in the heel & arch of the foot, especially with the first steps in the morning or after a period of rest
- Pain that worsens after prolonged standing or walking
- Swelling or tenderness around the heel or in the band of muscle from the heel to the toes, usually on the inside of the foot
How to Deal with Plantar Fasciitis
What I Did Right Away
Here are the things I did first to start my plantar fasciitis treatment, to relieve the pain and begin my healing process:
Rest and Avoid Overuse: Reduced activities that put pressure on the affected foot, like running, hiking, dancing or standing for long periods. That being said, I kept walking carefully for short lengths of time, because not moving around at all left my foot tight and immovable. I found that slow & careful walking was better than none at all.
Ice: Applying ice to the affected heel and arch for 15-20 minutes several times a day helped reduce inflammation and (eventually) relieve pain. I use a flexible ice pack that is extremely cold on the skin, so I always wrap it in a kitchen towel to protect my skin and to be able to keep the ice pack in place for the 15 minutes.
Anti-inflammatory Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help reduce inflammation and relieve pain. If you can’t take NSAIDs, you can also try acetaminophen for pain, but it won’t do much for swelling.
Stretching and Strengthening Exercises: Go easy on these! Try each one for a short period and then evaluate whether the exercise is helping. I found that these tended to work better after a few weeks of healing than they did immediately after the injury.
- Stretch the bottom of your foot by gently rolling it over a tennis ball or a foam roller. I cut a short piece of foam pipe insulation at first, because it was softer than the tennis ball. A piece of ‘pool noodle’ foam could also work.
- Calf stretches: Tight calves can contribute to plantar fasciitis, so gently stretching the calves can help.
- Plantar fascia focused stretches: Sit on the floor with your legs stretched out. Use a towel or a PT strap to pull your toes back toward you. First try doing this for a few seconds, then work up to holding for 20-30 seconds to stretch the fascia.
- Toe-tapping and pointing exercises: Strengthen the muscles around the foot by tapping your toes up and down while not supporting your body weight. Sit in a chair where your feet don’t touch the floor, as in a bar height stool or cross your leg with the injured foot over the other leg while sitting.
Other Suggestions for Plantar Fasciitis to Consider
I did not do these things, because they didn’t seem like they would help my particular situation. All injuries are different though, so I thought I’d mention them for completeness.
Night Splints: Wearing a splint at night that is designed for Plantar Fasciitis can keep your foot in a dorsiflexed position while you sleep, gently stretching the plantar fascia and Achilles tendon. There are several different designs.
Physical Therapy: A physical therapist (PT) can design a personalized stretching and strengthening program to help alleviate symptoms. Typically you will need to get a referral from your doctor to be able to see a PT. You should check your medical insurance first to see what is covered.
What Actually Helped – My Longterm Solution
Once I got through the first couple of weeks of recovery, I was told by one medical professional that I should throw away all my sandals and never wear any again for the rest of my life.
No!!! I live in sandals! There had to be a different solution.
I started doing research. I learned that I have very high arches in my feet, so I needed sandals and other footwear that are designed to support them. That is when I discovered The Walking Company. In 2017, they still had physical stores, and had a testing device where you could walk across a mat on the floor and the device would analyze the shape of your foot and where your foot put most of the pressure on the mat.
Not only did I have high arches, I would benefit from sandals that had a built-in Metatarsal Support, which is a ridge of material that supports the bones that are just behind your toes and it help your foot to not slide forward in the sandal.
They carry one particular brand of shoes, including a large number of sandal styles that have high arch support built into the footbed of the sandal. These sandals were clearly designed to be plantar fasciitis footwear. Some of the sandals are also offered with metatarsal support! The brand name is Abeo.
I bought my first pair of Abeo Sport sandals. They were just what I needed to support my foot while it was healing. The first thing I noticed was that the arch molded into the footbed exactly fit my foot and I felt a noticeable improvement in comfort as it was supported along the entire length of my foot.
To learn more about Abeo brand and all the types of footwear they carry, please see my article Best Shoes for Plantar Fasciitis: Abeo Sandals.
If you’d just like to view some of the styles online, here is a quick link for that:
The exact styles that I show in my pictures are not currently available on Amazon, so I am sending you to the Category page. That's actually good, because you'll be able to see a variety of styles, utilizing supportive footbeds.
Replacing Footwear
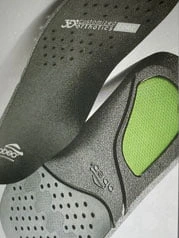
Next, I started replacing my regular walking shoes with Abeo choices. I had a pair of fairly new hiking boots that I liked, so I just replaced the inexpensive footbed that they had with an orthotic from Abeo that had both the high arch and metatarsal support.
Over the next five months, I took it easy on my feet and always wore good supportive footwear, and I gradually healed up. After that, I went back to all my regular activity levels: hiking, walking the dogs, gardening, and dancing. I have never had a recurrence of Plantar Fasciitis.
Hiking: Up to 6 miles on dirt/gravel/single track trail surface. Most hikes have up to 500 feet vertical variation over the hike.
Dancing: Up to three hours straight, including Swing dancing!
Gardening: A couple hours every spring, summer & fall morning. In cooler weather, I wear my hiking boots but when it is hot, I wear the sandals. Bonus: If the sandals get muddy, I can just hose them off! The materials stand up great to water.

When I am just out running errands or anything that doesn’t require the support of a strap behind my heel, I wear ‘flip flop’ styled sandals like this Balboa style. These have the high arch + metatarsal support built into the footbed.
Recovery Recap
It turned out that the same thing—always wearing supportive footwear—supported both my long-term recovery from injury and prevention of future injuries.
Proper Footwear: Wear shoes with good arch support and cushioning. Avoid walking barefoot on hard surfaces, as it can aggravate the pain.
Avoid High Heels: No heels taller than about 1.5 inches. If wearing wedges or boots, the difference in height between your heel and toe should not exceed 1.5 inches, even if the overall height exceeds that. Jamming all of your weight on the front of your foot is just bad physics. It will just catch up with you – even if you never get Plantar Fasciitis, other things go wrong like bunions and ‘hammer toe’.
Avoid High-Impact Activities: Running on hard surfaces or high-impact sports may worsen symptoms. Consider switching to low-impact exercises like swimming, walking or cycling.
Orthotic Inserts: Over-the-counter or custom-made insoles can provide extra arch support and help alleviate pressure on the plantar fascia. Custom made orthotics can run into the hundreds of dollars, but they are ‘lifesavers’ for people with difficult foot and leg length situations. I was fortunate that the premium orthotics from Abeo were the exact thing I needed for my foot structure – a much cheaper solution than custom-made orthotics.
I discuss more about these well-made insoles in my article Best Shoes for Plantar Fasciitis: Abeo Sandals. If you’d just like to see some of the choices, this quick link will take you to the Amazon selections.
This link takes you to all the Orthotic Insert choices that are currently on offer. The selections include inserts for different foot types and both men's and women's sizes.
About Metatarsalgia
Metatarsalgia is pain and inflammation in the ball of the foot. You may experience it in association with Plantar Fasciitis or on its own.
Metatarsalgia, literally ‘metatarsal pain’ and colloquially known as a stone bruise, is any painful foot condition affecting the metatarsal region of the foot. This common problem can affect the joints and bones of the metatarsals. — Definition from Wikipedia
Thanks for Featured Image go to (El Caminante) from Pixabay.